The Blood Stop and Go session included the following presentations:
1. Tor Audun Hervig: Pre-Hospital Use of Blood Products
2. Saif Ali: A large multicentre evaluation of massive hemorrhage protocol performance and compliance across adult and pediatric hospitals
3. Laura Green: Massive transfusion - can we agree on a definition?
4. Sakara Hutspardol: Comparison of ROTEM and Conventional Coagulation Tests in Identifying Trauma-Induced Coagulopathy During Massive Hemorrhage Protocol
5. Helen Elizabeth Haysom: Did critically bleeding RhD negative patients receive RhD matched RBCs? Data from the Australian and New Zealand Massive Transfusion Registry
MODERATORS: Arwa Al-Riyami and Jouni Lauronen
After the presentation, there was a questions and answers session of about 5 minutes, which is also included in the recording.
Abstract
A large multicentre evaluation of massive haemorrhage protocol performance and compliance across adult and paediatric hospitals
S Ali1, D Roque2, J Callum3, D Arnold4, N Li5, M Ly5, D Grimm6, A Singh1, K Murto7, K Pavenski8, L Da Luz9, A Petrosoniak10
1Michael G. DeGroote School of Medicine, McMaster University, Hamilton, 2Quality in Utilisation, Education and Safety in Transfusion (QUEST) Research Program, University of Toronto, Toronto, 3Department of Pathology and Molecular Medicine, Queen's University, Kingston, 4Faculty of Health Sciences, Division of Hematology & Thromboembolism, McMaster University, Hamilton, 5University of Calgary, Calgary, 6Queen's University, Kingston, 7Department of Anesthesiology & Pain Medicine, CHEO Research Institute, University of Ottawa, Ottawa, 8Department of Laboratory Medicine, St. Michael's Hospital, 9Sunnybrook Health Sciences Centre of Surgery, 10Department of Emergency Medicine, St. Michael's Hospital, University of Toronto, Toronto, Canada
Background: Massive Haemorrhage Protocols (MHPs) allow for rapid and standardised delivery of blood components to patients with critical bleeding. To address variability of MHP performance and standardise the approach to massive haemorrhage, the Ontario Regional Blood Coordinating Network, released an MHP toolkit developed by experts, comprising 42 evidence-based principles and nine quality metrics. We conducted a multicentre cohort study to evaluate compliance with the quality metrics in practice.
Aims: To evaluate MHP performance across adult and paediatric patients in Ontario, Canada including the impact of timely haemostatic and transfusion therapies, and blood product wastage.
Methods: We reviewed consecutive MHP activations across 15 hospital sites from January 01, 2019 to July 31, 2022 (n = 1844), and collected demographic data, outcomes, and MHP quality metrics using an electronic data collection tool (REDCap®). The primary objective was to measure overall MHP performance using a validated MHP case score, calculated as a proportional score out of a maximum of nine quality metrics. Not all activations could be evaluated for all nine metrics (e.g., timely patient transfer out was not evaluated at all tertiary care centres). Categorical data were analysed using Pearson's Chi Squared test and Fisher's exact tests. Logistic regression analyses were conducted to identify risk factors for in-hospital death at 24 h and up to 28 days. Appropriate MHP activations were defined as >6 red blood cell (RBC) units (>40 mL/kg of RBCs in paediatric patients) within 24 h from the time of activation or haemorrhagic death in the first 24 h.
Results: We analysed MHPs for patients <18 years (n = 86, 5%), 18–65 years (n = 1228, 66%) and >65 years (n = 530, 29%); 1250 (68%) were male. Most MHP activations occurred in the emergency department (51%) and were triggered by trauma related injuries (45%). In-hospital 28-day mortality was 37% (n = 679) overall, and highest among patients >65 years (47%) compared with younger adults (32%) and children (38%). Of all MHP activations, 40% were considered inappropriate and 25% were associated with blood product wastage, especially plasma (717 units). In multivariate analysis, improved survival was associated with a haemoglobin (Hgb) level above 60 g/L for first 24 h but below 110 g/L at 24 h, patient temperature ≥35°C at MHP termination, and administration of tranexamic acid (TXA) within 1 hr (Table 1).
PA02-L02 - Table 1: Multivariate logistic regression analysis for the association between quality metric performance and death
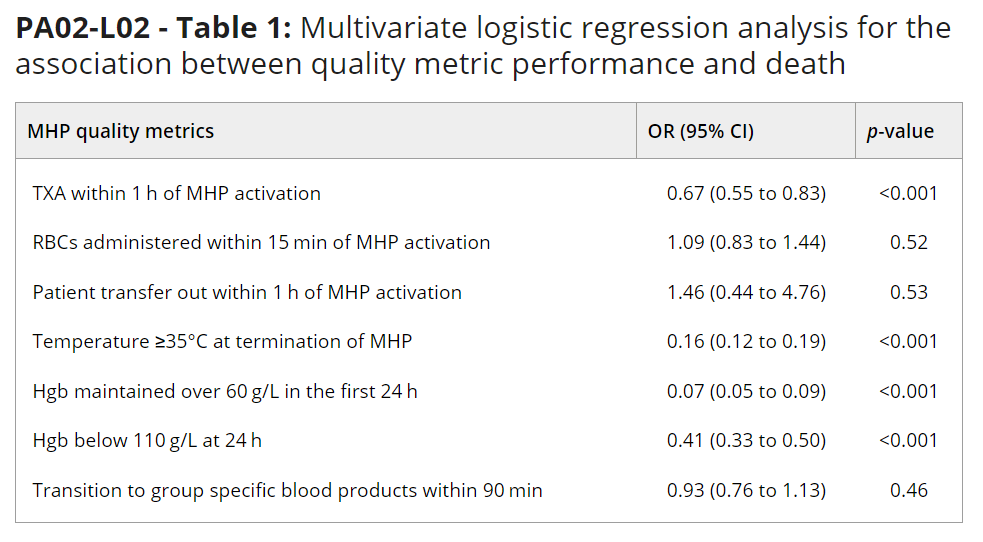
Summary/Conclusions: In this large, multicenter study, mortality from massive haemorrhage was highest among patients >65 years, necessitating a better understanding of how to optimise care for these patients. MHP over activation and blood product wastage were common. Administration of TXA within 1 h, haemoglobin levels above 60 g/L (in the first 24 h) but less than 110 g/L (at 24 h), and patient temperature ≥35°C were associated with improved survival.






